ATLANTA — Thousands of Georgians risk losing Medicaid coverage during the Medicaid redetermination process, also known as Medicaid unwinding.
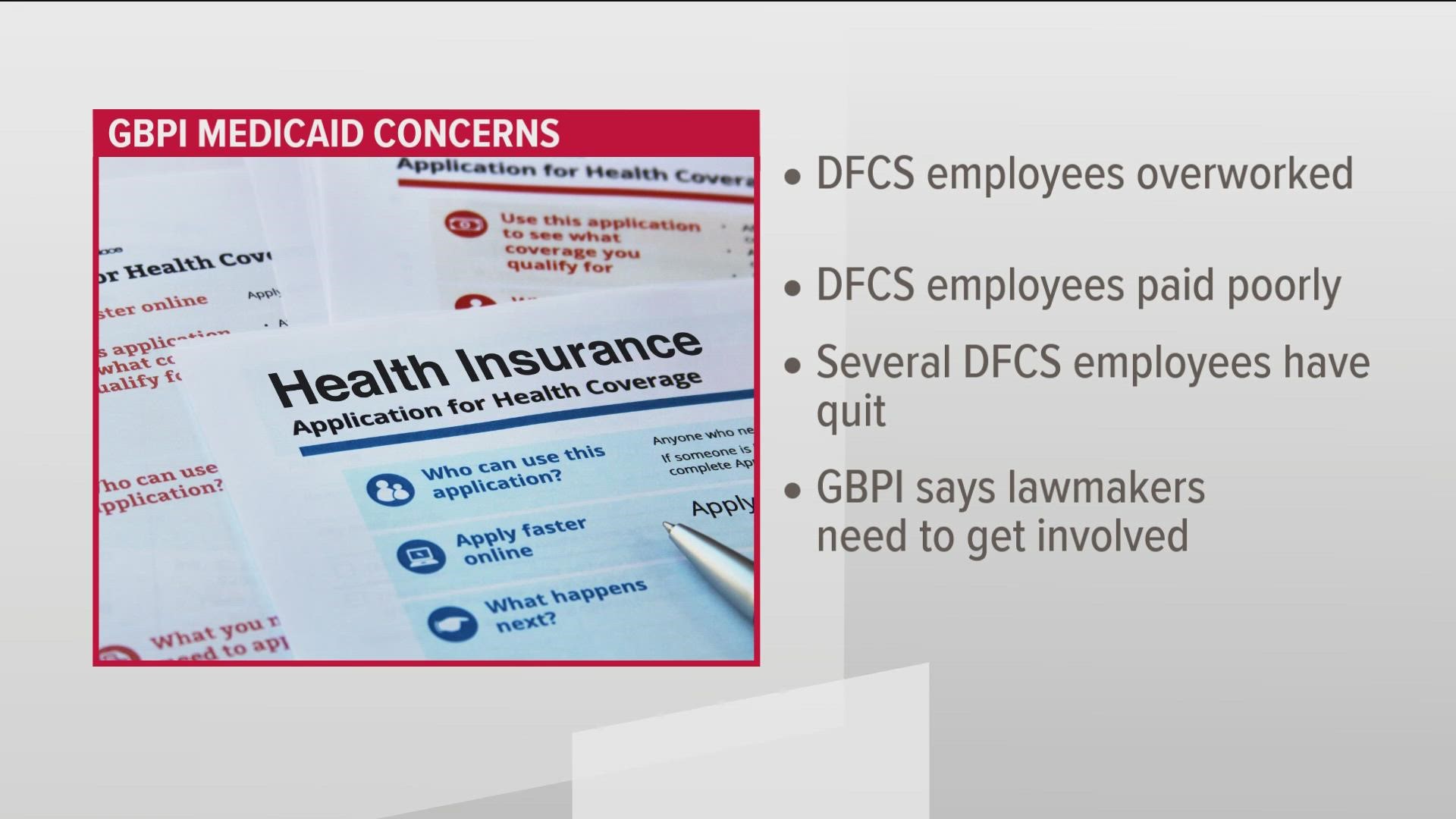
The Georgia Budget and Policy Institute (GBPI), an Atlanta-based nonprofit, which analyzes tax policies and proposed budgets in Georgia, reports that the Georgia Division of Family and Children Services (DFCS) staff are unprepared to handle the unwinding process.
According to the GBPI, high workloads, long hours and insufficient pay put a strain on DFCS agency staff.
"Many DFCS frontline workers have quit. With Medicaid unwinding just weeks away, these problems are sure to worsen as caseloads increase to unprecedented levels," GBPI Director of Economic Justice Ife Finch Floyd said.
Leah Chan, a Senior Health Analyst at GBPI, said the nonprofit is worried about the potential loss of coverage if state legislators don't intervene.
Millions of Georgians to have Medicaid coverage re-evaluated
In Georgia, roughly 2.7 million people with Medicaid coverage will be reevaluated by the Department of Community Health and the Department of Human Services.
The GBPI estimated that 545,000 Georgians could lose coverage during Medicaid unwinding. GBPI estimated that roughly half would lose coverage due to avoidable procedural reasons.
"Almost half will lose coverage, not because they're no longer eligible, but because of a potentially avoidable procedural reason, like the form gets sent to the wrong address or it's sent to their house, but it's in a language that they don't speak," Chan explained.
Those most at risk for losing Medicaid are mothers past their one year of postpartum coverage, young adults aging out of Medicaid and peach care, and children.
Chan explained children, specifically Black and Latinx children have a higher risk of losing Medicaid coverage due to an avoidable procedural reason.
Medicaid eligibility redetermination explained
During the COVID-19 pandemic, the U.S. Congress passed the Families First Coronavirus Response Act in March 2020.
As listed on DHS' website, the law gave states a temporary 6.2% federal funding increase if states provided continuous coverage for people on Medicaid starting March 18, 2020, through the end of the month – when the federally declared public health emergency expires.
On April 1, 2023, the continuous Medicaid coverage requirement will start to unwind. Beginning on April 1, all states will have 14 months to reprocess those with Medicaid coverage eligibility.
All Medicaid redeterminations must be completed in Georgia by May 31, 2024.
"This will really be an unprecedented healthcare event here in our state. We've never had to reprocess the eligibility of this many folks in this amount of time," Chan said.
What Georgians with Medicaid coverage should do
The GBPI urges Medicaid recipients to take action and visit its online Georgia Gateway account, the state government's web portal, to access assistance programs.
Medicaid recipients must ensure all their information is updated, including phone number, address, job or income, and the number of people in their household.
DHS' website encourages enrollees to select "Email" notifications for the fastest alerts regarding Medicaid enrollment updates.
"Once the unwinding starts on April 1st, be checking your email, your mailbox, and making sure you're keeping on top of whether you've gotten, you know, the different paperwork you must complete during the process," Chan explained.
Chan urged all Georgians to contact their state representative and state senator and ask to amend the state budget for 2023 and 2024.
According to the GBPI, the amended FY 2023 and FY 2024 budgets should include:
- Sub-grants to community-based organizations who can serve as trusted messengers and provide localized and culturally appropriate education and outreach, and where possible, assist with re-enrollment or transitions to marketplace coverage.
- Retention bonuses and/or pay raises for Department of Human Services’ Office of Family Independence staff involved in benefits eligibility processing.
"There's so much that we can do as Georgians to really advocate that our state legislature does everything they can before the end of this session to make sure that our state agencies have what they need to process a successful unwinding that does minimal harm and allows Georgians to stay covered," Chan said.
The end of Georgia's regular session is Thursday, March 30.
For more information about the Medicaid unwinding process, click here.